Fibromyalgia
What is Fibromyalgia?
Fibromyalgia is a chronic disorder that is characterised by widespread pain and tenderness throughout the musculoskeletal system. People may experience sleep disturbance, fatigue, anxiety and depression, and a range of other symptoms. Although Fibromyalgia is considered like arthritis, affecting muscles and joints, it does not cause damaging inflammation to the body. The medical field still do not understand the direct cause of the disorder, meaning there is no cure. Fibromyalgia may be a life-long illness which fluctuates in severity of symptoms, with possible periods of remission. Medication, diet, physical exercise, stress, weather, sleep, mental health support and alternative therapies may affect the severity of symptoms. Up to 1 in 20 Australians suffer from Fibromyalgia. Women between the ages of 35 and 55 are more likely to develop the condition.
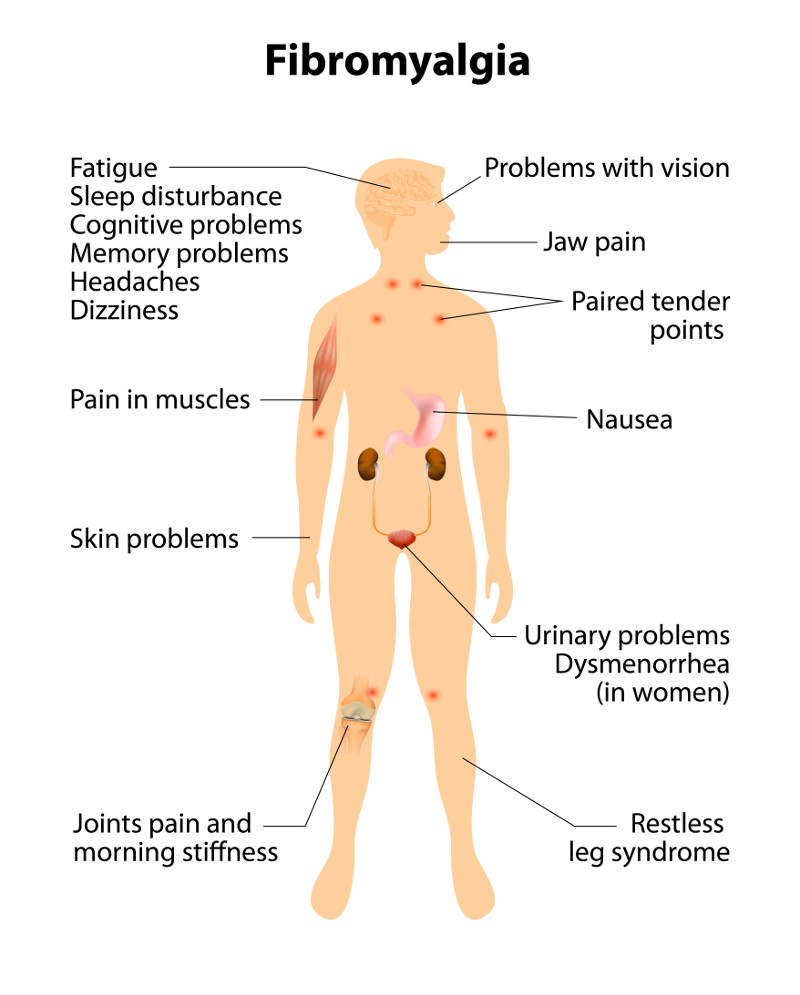
What are the Symptoms of Fibromyalgia?
- Widespread pain and tenderness throughout the body which varies in feeling, including dull, sharp, burning, throbbing or stabbing
- Muscle stiffness which is more prevalent at the beginning and the end of the day
- Insomnia and nonrestorative sleep
- Overwhelming fatigue resulting in apathy and lethargy
- Inability to concentrate, 'brain fog', and memory problems
- Psychological symptoms such as anxiety, depression and suicidal thoughts
- Headaches and migraine
- Paraesthesia (prickling, numbness and tickling in extremities)
- Irritable bowel syndrome
- Dizziness, vertigo
- Sensitivity to loud noises and bright lights
- Restless leg syndrome
- Sensitivity to temperature
People with Fibromyalgia may also have other conditions, including:
- Chronic fatigue
- Cardiac disorders
- Psychiatric disorders
- Headache/migraine
- Hypertension
- Premenstrual syndrome, dysmenorrhoea and endometriosis
Pain Symptoms
Pain is typically widespread, although different regions of the body may be more painful at various times with varying intensity. There may be a history of chronic local pain, such as lower back pain before symptoms become more widespread 1. Pain is described as persistent aching, burning, stabbing, soreness and tenderness. Physical activity can intensify pain, although sharp, spontaneous spasms of pain can occur without physical activity. Muscles may feel tense and knotted with a feeling of tenderness, where light touch or pressure causes severe pain. The pain is often disabling, affecting the quality of life of people living with Fibromyalgia. Managing daily routines such as work and household chores can be challenging to fulfil. Pain and muscle stiffness is often worse in the morning and at night. Stress, activity and cold or humid weather can cause 'flare ups' where pain becomes more severe and other symptoms intensify 2.
Stiffness starts in the morning; however, it does not improve throughout the day 1.
Fatigue
Fatigue is another disabling feature of Fibromyalgia, which is generally worse in the morning and evening. Fatigue affects the patient's ability to function throughout the day. Light physical or mental activity often causes exhaustion and recovering for activities can take longer 3.
Non-restorative Sleep
Many patient's do not feel refreshed after a night's sleep, describing feeling tired and drained, which affects their ability to function throughout the day. Some patient experience waking several times a night. Poor sleep quality can exacerbate symptoms of Fibromyalgia, where the production of serotonin and human growth hormone can be interrupted, important hormones which moderate pain and stress levels 3. With poor sleep comes a less effective immune system, leaving the body susceptible to infection. Mood swings and irritability can also be the result of poor sleep. Restless leg syndrome is common among people with Fibromyalgia, causing pain in the lower limbs at night, further contributing to poor sleep quality 1.
Psychological and Emotional Symptoms
Depression and anxiety may result from the symptoms of Fibromyalgia, including widespread pain, fatigue and the long-term prognosis of the disorder. In others, depression may pre-date the onset of widespread pain and fatigue. The onset of widespread pain may have occurred at a time when the patient was experiencing low mood. Anxiety often co-exists with depression in patients with Fibromyalgia. Anxiety symptoms may include dizziness, shortness of breath, heart palpitations, and excessive sweating 1.
Brain fog or 'fibrofog' is a common symptom, where patients have difficulty with memory, retaining new information, problem-solving and mental arithmetic. 'Fibrofog' may last a few days at a time, affecting quality of life, functionality at work and completing daily tasks. Some patients describe this as being worse than the pain 3.
How is Fibromyalgia Diagnosed?
Fibromyalgia is complex and can be challenging to diagnose. There are no laboratory tests available, so doctors need to rule out other medical conditions before diagnosing a patient with Fibromyalgia. The condition is diagnosed by assessing the severity, location and history of widespread pain. There are 19 points on the body that are assessed for tenderness and pain 2. Widespread pain which lasts longer than three months is typically part of the diagnosis criteria. Symptoms that include fatigue, lack of refreshing sleep, cognitive impairments, abdominal discomfort, headache and depression are also considered 4. The doctor must rely on the patient's experiences of symptoms and patients can sometimes not be believed or receive a mental health diagnosis 5. Patients can see several doctors before receiving a Fibromyalgia diagnosis, causing frustration and anxiety.
Who Gets Fibromyalgia?
2-5% of the population are diagnosed with Fibromyalgia, of which 80-90% are women ranging from young to middle-aged, with the average age ranging between 35-55 years old. Men and children are diagnosed at a far lesser rate.
What is the Prognosis?
Fibromyalgia does not increase the mortality rate or deteriorate organ function. Widespread pain is experienced as long-term; however there may be periods of remission.
What Causes Fibromyalgia?
Current research suggests that the way pain is processed in the central nervous system (found in the brain and spinal cord) is abnormal in people with Fibromyalgia. The condition can be described as the volume of pain registered in the brain being turned up too high. Neurotransmitters in the brain that process pain and other stimuli are shown on imaging to be extremely sensitive 2. Levels of Serotonin, a neurotransmitter responsible for diminishing pain and regulating sleeping patterns, are decreased 3. This may be due to inheriting certain genes. Although genes may play a role in developing the disorder, environmental factors may trigger development of the condition. Fibromyalgia may be triggered by physical, or emotional stress; such as an underlying medical condition, a physical trauma, such as a car accident, or psychological trauma, such as abuse. Post-traumatic Stress Syndrome (PTSD) is common in people with Fibromyalgia 6. In a study conducted of 77 patients (aged 22-70) who diagnosed with Fibromyalgia, 57% also met the criteria for PTSD, suggesting that there is an overlap between the two conditions 7. Underlying infection or autoimmune conditions can be a risk factor for developing Fibromyalgia, including rheumatoid arthritis and lupus.
What Causes Pain in the Muscles?
People who suffer muscular pain usually have an insufficient supply of energy to the muscle. A phosphate called Adenosine Triphosphate (ATP) is responsible for supplying this energy. With an inadequate amount of ATP, the muscle tissue is unable to relax after contracting, causing the muscles to stay in a 'shortened position', which creates tension in the muscle and fascia. Blood flow to affected tissue becomes limited, which depletes oxygen levels to the tissue, resulting in muscular pain.
How is Fibromyalgia Treated?
There is no treatment for Fibromyalgia, although with the use of multiple therapies, symptoms can be relieved. Medication, alternative therapies and lifestyle usually achieves the best outcomes.
Non-Drug Therapies
Research shows that physical activity, particularly aerobic exercise, is the most effective treatment for Fibromyalgia 8. Exercises that stretch and strengthen muscles are also ideal such as walking, swimming and water aerobics. Low impact exercise will not be harmful. Start exercise slowly at a low impact pace to incorporate it into your daily routine, then build up your activity over time. Activities such as Thai Chi and Yoga are beneficial and incorporate mindfulness and breathing strategies that are beneficial to reduce stress, anxiety and the effects of pain.
Cognitive Behavioural Therapy
Cognitive Behavioural Therapy is a useful psychological treatment 9 as it focuses on how thoughts and behaviours can affect pain and other symptoms of Fibromyalgia.
Complementary Therapies
Complementary therapies such as massage therapy, acupuncture and chiropractic therapy can be useful to manage symptoms of Fibromyalgia.
Self-Care
Self-care may give patients a sense of control over their condition as well as stress relief which may decrease 'flare ups'. Apart from the techniques listed directly above, some patients find the following strategies helpful.
Sleep Strategies
Sleep Strategies including setting a regular sleeping pattern, avoid day time napping, guided imagery relaxation technique, stimulus control therapy and sleep hygiene can help clients fall asleep or get back to sleep.
Pacing and Planning
Pacing and Planning involves planning your day and balancing the amount of activities you do, which may mean asking others for help to complete essential tasks.
Social Support
Social Support is vital for mental health outcomes. It might include, a Fibromyalgia support group, talking to a friend, counselling. Share information with friends and family so they can understand how best to support you.
Relaxation
Relaxation could include meditation, resting, taking a warm bath, journaling, breathing techniques, biofeedback and the use of essential oils.
Good Nutrition
Good Nutrition is important to increase energy and maintain general wellbeing. A few studies have shown that diets high in raw vegetables can minimise pain. Maintaining a healthy weight can also decrease pain and increase energy levels.
Pharmaceutical Medications
In Australia, approved antidepressants that help to control pain response levels include; Amitriptyline, Duloxetine and Milnacipran. Not all patients will benefit, and side effects may be experienced more profoundly by different people. Always consult your doctor about the benefits and risks of these medications.
Pregabalin is another approved drug in Australia that works as a nerve blocker, which can limit the activity of nerve cells, which can decrease the transmission of pain. The side effects of this drug may cause dizziness, drowsiness and weight gain.
Research recommends that opioids should be avoided as they can actually increase pain sensitivity in people with Fibromyalgia.
Over the counter anti-inflammatories such as ibuprofen and naproxen are not helpful for Fibromyalgia. Anti-inflammatories may treat related pain triggers such arthritis if this diagnosed in addition to Fibromyalgia.

Can Massage Help People with Fibromyalgia?
Studies show that myofascial release massage therapy has significant positive effects on pain and moderate effects on anxiety and depression at the end of treatment. Myofascial release can improve fatigue, stiffness and quality of life 8.
Fascial tissue surrounds and supports muscles in the body. Pain with Fibromyalgia usually originates in "trigger points" which are specific points within the fascial tissue. Myofascial release focuses on reducing pain by easing the tension and tightness in the trigger points.
Healthy fascial tissue should feel pliable and elastic. The therapist will feel for stiff or tightened areas and stretch the area that feels rigid using gentle, manual pressure. Myofascial release helps to decrease fibromyalgia pain and stiffness by elongating muscle fibres.
Massage increases joint mobility, circulation of blood flow and oxygen to the muscles. It helps to eliminate built-up toxins within the tissue. Massage decreases heart rate and stress hormones and increases endorphins which act as natural pain killers. By reducing pain sensitivity and anxiety levels in people with Fibromyalgia, myofascial release can improve sleep quality and physical function 10.
People with Fibromyalgia should consult their physician before any massage therapy. An intake assessment will allow the client to inform the massage therapist of their symptoms related to Fibromyalgia. The client can discuss their experiences of pain, triggers, medications, allergies and current management of symptoms. The massage therapist will check-in with the client before each session to get an understanding of any changes to the client’s symptoms, medications, therapies and pain sensitivity. It is recommended to only receive massage with gentle pressure to start with as the muscles may be sensitive. Sensitivity to pain may improve over a few treatments, allowing the therapists to apply deeper pressure to muscles, joints, and ligaments. Massage for Fibromyalgia can vary from light stroking to deeper pressure depending on the needs of the client. Communication between the client and therapist is essential as clients with Fibromyalgia experience good and bad days with symptoms of the condition.
When used as part of a holistic approach to manage symptoms of Fibromyalgia, massage is a beneficial complementary therapy.
References
1. Choy E, author. Fibromyalgia Syndrome. Second ed. Oxford: Oxford University Press; 2015.
2. Sugerman DT. Fibromyalgia. JAMA. 2014;311:1577-1577.
3. Robertshawe P. Treating fibromyalgia with massage. Journal of the Australian Traditional- Medicine Society. 2007;13:151.
4. Wolfe, D. J. Clauw, M.-A. Fitzcharles et al., “Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR preliminary diagnostic criteria for fibromyalgia,” Journal of Rheumatology, vol. 38, no. 6, pp. 1113–1122, 2011.
5. Armstrong FE. Quality of life for patients with fibromyalgia. Nursing Made Incredibly Easy!. 2019;17(6):20–26. doi: 10.1097/01.NME.0000585080.89312.18.
6. Carmassi, C. Manni, G. Cipollone, C. Tagliarini, M.T. Avella, C. Portulano, G. Massimetti, C. Conversano, L. Bazzichi, C. Gesi, L. Dell’Osso. DSM-5 PTSD and Post-Traumatic Stress Disorder Spectrum in patients with fibromyalgia: Possible correlations with subthreshold autism spectrum?,European Psychiatry,Volume 41, Supplement,2017,Page S722,ISSN 09249338,
7. Splete, H. "PTSD overlaps fibromyalgia. (Clinical Capsules)." Clinical Psychiatry News, Oct. 2002, p. 78. Gale General OneFile.
8. Yuan SLK, Matsutani LA, Marques AP. Effectiveness of different styles of massage therapy in fibromyalgia: A systematic review and meta-analysis. Manual Therapy. 2014;2015;20:257-264.
9. Bernardy K, Füber N, Köllner V, Häuser W. Efficacy of cognitive-behavioral therapies in fibromyalgia syndrome - a systematic review and metaanalysis of randomized controlled trials. The Journal of rheumatology. 2010;37:1991
10. Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J, Aguilera-Manrique G, Quesada-Rubio JM, Moreno-Lorenzo C. Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evidence-based complementary and alternative medicine : eCAM. 2011;2011:561753-9.


